What Is Pancreatitis?
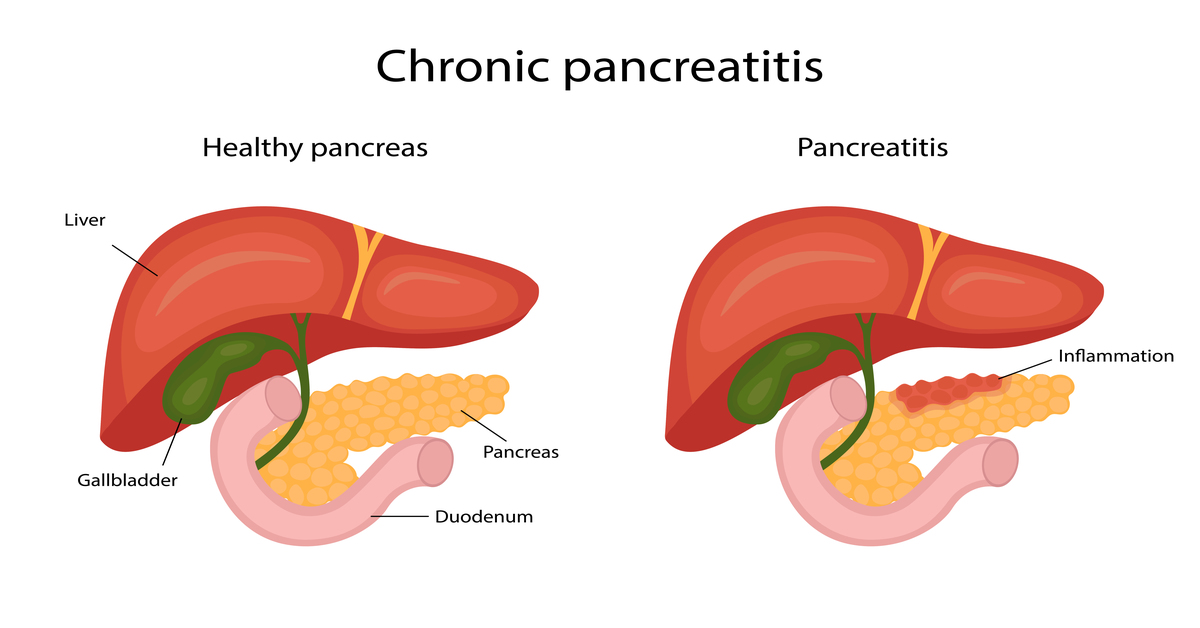
Inflammation of the pancreas is a characteristic of pancreatitis.
The pancreas is a large gland that is situated beneath the stomach and next to the small intestine. Your pancreas does two main things:
- It releases powerful digestive enzymes into your small intestine to help you digest food.
- It releases insulin and glucagon into your bloodstream. These hormones help your body control how it converts food into energy.
When digestive enzymes start to function before your pancreas releases them, the pancreas may become injured.
What Are the Types of Pancreatitis?
There are two main types:
- Acute pancreatitis is a quick, transient inflammation. It can cause anything from minor pain to a serious, life-threatening condition. In severe cases, acute pancreatitis can cause bleeding, tissue damage, infection, and cysts. Acute severe pancreatitis can also harm other vital organs such as the heart, lungs, and kidneys.
- Chronic pancreatitis is long-lasting inflammation. After a bout of acute pancreatitis, it occurs most frequently. The prolonged consumption of large amounts of alcohol is another major factor. Heavy drinking can harm your pancreas, although it might take years before you have severe pancreatitis symptoms.
What Are the Signs & Symptoms of Pancreatitis?
1 Pain in the upper abdomen- The pain often radiates to the back.
2 Nausea and vomiting
3 Fever 4 Weight loss, greasy stools, and diarrhea may be symptoms of chronic pancreatitis. 5 Jaundice (due to gallstone)
6 High pulse rate
7 Bloating & fullness of the abdomen
What Are the Pancreatitis Causes and Risk Factors?
CAUSES OF PANCREATITIS:-
1 Alcohol
2 Gallstone
3 Obesity
4 Smoking
5 Genetic disorders
6 Hypertriglyceridemia 7 Hypercalcemia
8 Hyperparathyroidism
9 Abdominal trauma
10 Some Medications
11 Infections—Mumps
12 Junk food & sedentary lifestyles
13 Malnutrition
14 Autoimmune
How Is Pancreatitis Diagnosed?
Diagnosis:-
1. Blood reports:-Amylase, Lipase, Ionized calcium, LFT, Triglyceride
2. USG abdomen& pelvis
3. CECT abdomen & pelvis (after 72-96 hours from onset of pain)
4. Endoscopic retrograde cholangiopancreatography. The bile and pancreatic ducts are examined during the surgery. Uses an endoscope in addition to X-rays. An endoscope is a flexible, lit tube with a camera attached to it. ERCP is a procedure that gastroenterologists use to diagnose and treat conditions involving the liver, pancreas, gallbladder, and bile ducts. Mainly help in the diagnosis of biliary pancreatitis. 5. An endoscopic ultrasound (EUS) helps to diagnose diseases of the digestive tract. Endoscopy, which makes use of a thin, flexible tube with a camera and light at the end, is combined with another type of technology. Ultrasound uses high-frequency sound waves to create detailed pictures of internal organs. It helps to diagnose chronic pancreatitis, gallstones, tumors in & around the digestive system, and lesions in the abdomen. 6. MRCP:- A magnetic resonance cholangiopancreatography (MRCP). It is an imaging examination to look at your biliary and pancreatic systems. A dye is injected into your veins through an intravenous (IV) line for this test. It helps to clear the image of organs, veins & ducts. It helps to diagnose Pancreatitis, Biliary duct cancer, biliary stricture, and choledocolithiasis.
How Is Pancreatitis Treated?
Treatment
- Hospitalization
- Keep the patient fasting? Once pancreatitis is controlled, he can be started on clear liquids, bland food, and a gradually normal diet.
- IV fluids, IV analgesics.
- Treating the cause of Pancreatitis.
- ERCP to remove bile duct obstructions
- Cholecystectomy in case of gall stones causing Pancreatitis.
- In the event of pancreatic necrosis, pancreatic surgery.
- Avoid alcohol consumption
What is a complication of pancreatitis?
Complications:-
- Pseudo cyst
- Infection
- Diabetes
- Malnutrition
- Breathing problems
- Kidney failure
- Pancreatic cancer
How Do You Prevent Pancreatitis?
Prevention:-
1 Avoid alcohol consumption & smoking
2 Do not neglect Gallstone
3 Healthy lifestyles
4 Periodic health checkups
5 Reach out to specialists (Gastroenterologists)
Author :- Dr Sanjiv Haribhakti
M.Ch. GI Surgeon of Western India
Kaizen Hospital